Pathology
Cardiac Tamponade & Pericardial Effusion
cardiac tamponade: Just the facts!!!
Give Volume! Preload dependent!
Tamponade can occur in relatively small effusions (150cc) when fluid accumulates rapidly
Echo findings suggestive of cardiac tamponade physiology include:
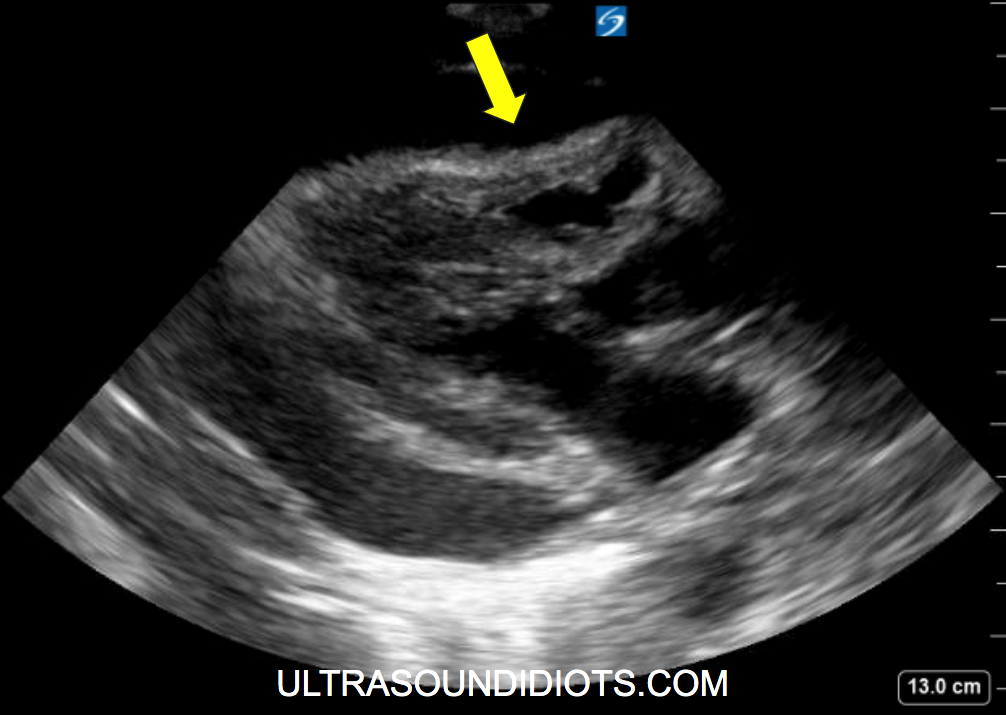
RA Collapse during systole. (Fig 1a, 1b)
RV free wall diastolic collapse.
Look for irregular movement of the RV free wall. (Fig 1c, 2b, 2c). Normal RV function, with and without effusion can be seen on figures 2a and 2b.
Temporal resolution:
Freeze clip and isolate image in diastole with mitral valve open. (Fig 1d)
Use M-Mode sampling through RV free wall and Mitral Valve. Typically done in PLAX, but can be any view. (Figure 1e)
Pulsus Paradoxus by echo (Fig 1f)
DIlated IVC (fig 1g)
If the effusion does not demonstrate clear findings suggestive of tamponade then the provider should consider other causes of shock/instability !!
Cardiac Tamponade and Pericardial Effusion
In order to efficiently and effectively care for ill and critically ill patients it is imperative that the POCUS provider be comfortable with limited echocardiogram image acquisition and the diagnostic findings associated with pericardial effusion causing cardiac tamponade. In the most unstable medical and trauma patients, current ACLS and ATLS guidelines note that Cardiac Tamponade must be considered highly in the differential. As a consequence, limited echo views are a major component of the diagnostic ultrasound protocols (E-FAST and RUSH). Moreover, limited echocardiography can also quickly eliminate diagnostic uncertainty in the ill-but-stable patient in which pericardial effusion is high on the differential. Provided below is a review of point of care ultrasound as it applies to the assessment of pericardial effusion and cardiac tamponade.
Pericardial Effusion (2,5)
A pericardial effusion is an accumulation of fluid within the pericardial sac and can be detected in echocardiography when volume exceeds 15-35cc. Cardiac tamponade occurs when the intrapericardial pressure, caused by fluid accumulation, increases to the point at which it impairs cardiac filling (diastolic function) and decreases cardiac output. The development of cardiac tamponade is a dynamic process and it is not dependent on the specific size of the effusion but rather the intrapericardial pressure. Consequently, asymptomatic pericardial effusions can vary greatly in size and may even exceed 1000 cc without causing tamponade physiology. In contrast, tamponade can occur in acute effusions with as little as 150cc. The size of an effusion is often reported by gross assessment but can be graded by measurement as:
Grade 1 / Small = echo-free space in diastole <10mm
Grade 2 / Moderate = echo-free space in diastole 10-20mm
Grade 3 / Large = echo-free space in diastole >20mm
Parasternal Long Axis views of pericardial effusion
parasternal short axis views of pericardial effusion
Apical Views of pericardial effusion
subcostal views of pericardial effusion
Risk factors for Pericardial Effusion and cardiac tamponade (2
Pericardial effusion and cardiac tamponade may be associated with the following diseases/conditions:
Infection (viral, Bacterial, Fungal)
Neoplasm
Drug Induced
Pericarditis
Myocardial Infarction (Dressler Syndrome)
Connective Tissue Disease
Uremia, Hypothyroid (Myxedema)
Iatrogenic
Trauma
Aortic Dissection
Idiopathic
When to use limited echocardiography to evaluate for pericardial effusion
Cardiac tamponade is considered a “must-not-miss” diagnosis in unstable medical and trauma patients. Unfortunately, in the absence of peri-arrest, its diagnosis is often delayed unnecessarily. This is largely due to the fact that clinically significant non-traumatic pericardial effusions can often present with nonspecific symptoms such as tachycardia, dyspnea, chest pain, or fatigue. In order to efficiently utilize time and resources, the following approach should be considered by providers when deciding to perform a limited echocardiogram to evaluate for effusion.
Perform a limited echocardiogram and other required limited studies in all unstable trauma and medical patients. (EFAST/RUSH) protocols.
Perform a limited echocardiogram and other required limited studies in all undifferentiated ill stable patients with risk factors for pericardial effusion. (See risk factors above)
Perform a limited echocardiogram and other required limited studies in all undifferentiated ill stable patients that have the following findings during initial workup:
Chest Trauma
New or changing cardiomegaly on CXR. (links to the details)
Unilateral left pleural effusion on CXR (links to add)
Reduced ECG amplitude +/- electrical alternans
CT or other imaging findings suggestive of pericardial effusion
Strongly Consider a performing limited echocardiogram and other required limited studies in all undifferentiated ill stable patients that have the following history:
Chest Trauma
Unexplained Syncope
Unexplained Dyspnea
Unexplained Chest Pain
Unexplained Tachycardia
Potential False Positives (Mimickers)
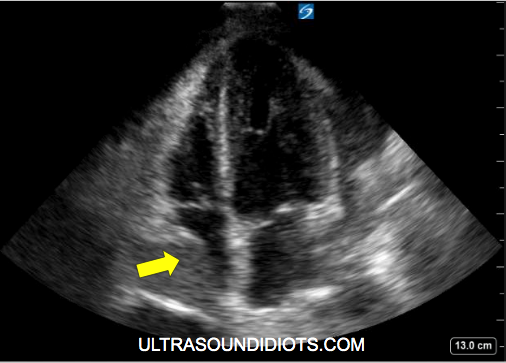
Pericardial fat pad. See Figures 3a, 3b. Note the adipose tissue within the pericardium. Note hyper-echoic densities that move with the RV free wall.
Left pleural effusion. See Figures 3c, 3e, 3f, 3g. Note that Figure 3d is actually an extremely large pericardial effusion with a trace pleural effusion posteriorly.
Hematoma
Very large left atrium
Left ventricular pseudoaneurysm
Hiatal hernia
Inferior left pulmonary vein
Cysts
Foramen of Morgagni hernia (congenital diaphragmatic hernia)
The diagnosis of a symptomatic large pericardial effusion should not be made five hours after initial assessment with a CT chest.
LINK TO ALL IMAGES/CLIPS
LINK TO PAGE BUILD
References
Otto CM. Textbook of Clinical Echocardiography. 5th ed. Philadelphia, PA: Elsevier Saunders; 2013.
Maisch B, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004 Apr;25(7):587-610.
Khandaker MH, Espinosa RE, Nishimura RA, et al. Pericardial Disease: Diagnosis and Management. Mayo Clinic Proceedings. 2010;85(6):572-593. doi:10.4065/mcp.2010.0046.
Ariyarajah V, Spodick DH: Cardiac tamponade revisited: A postmortum look at a cautionary case, tex heart inst J. 2007; 34(3):347-351
Ma J, Mateer J. Emergency Ultrasound. 4th ed. McGraw-Hill; 2021
CXR and Pericardial Effusions (finish the review)